Yuji Atarashi Tavares 1, Maycon Cristian Gomes de Paula 2, Gustavo Andrade Godoi Moreira 3, Augusto Castelli Von Atzingen 4
Resumo
Acute mesenteric ischemia is a relatively rare condition, representing approximately 1% of every acute abdomen cases. We report a case of a 93-year-old woman, complaining of diffuse abdominal pain in the last two days. Diagnosis was established by CT, which revealed an occlusion in the superior mesenteric artery. Treatment options for this condition are open surgery or endovascular repair. However, none of these approaches were performed due to patient’s clinical status.Dados do caso
Feminino, 93 anos.
Palavras chaves
Abdomen, Acute, Mesenteric Ischemia, Emergency Medicine.
Histórico Clínico
A 93-year-old woman presented to the emergency department with a 2-day history of sudden and diffuse abdominal pain. Physical exam revealed confusion, tachypnea and tachycardia. The abdomen was tense, distended, and diffusely painful on palpation but without peritoneal irritation signs. The patient underwent an electrocardiography, which revealed atrial fibrillation with rapid ventricular response, and a CT, that established the diagnosis of acute mesenteric ischemia (AMI) with portal venous gas. Afterwards, the patient had a decrease in her level of consciousness, followed by cardiopulmonary arrest and death.
Achados Radiológicos
An IV contrast-enhanced abdominopelvic CT was performed. An occlusion in the superior mesenteric artery was observed in the arterial phase, coronal plane, and confirmed the diagnosis of acute mesenteric ischemia (figure 1). A coronal image, in the portal venous phase, shows gaseous distention of intestinal loops, air inside the superior mesenteric vein and pneumatosis intestinalis (figure 2). An axial image, in the portal venous phase, revealed air in the portal vein, and the diagnosis of portal venous gas was done (figure 3).
Discussão
Acute mesenteric ischemia (AMI) is a relatively rare condition, representing approximately 1% of every acute abdomen cases. [1]. By the other hand, mortality rate remains high, ranging from 60% to 80%. The main cause of AMI is mesenteric arterial embolism (40-50%). [1,2]. Patients typically present acute abdominal “pain out of proportion to the examination” that can be associated with nausea, vomiting and changes in mental status. Further, the collapse of the mucosal barrier contributes to bacterial translocation, which leads to sepsis and multi-organ failure. [1-3]. Although portal venous gas (PVG) is in general uncommon in acute abdominal conditions, it can be observed in several disorders, including necrotizing enterocolitis, gastric ulcer and AMI, the latter of which is the most common cause of PVG in adults (43%). Because of its various causes, PVG can be of variable significance. However, when secondary to AMI, it is often associated with severity. [2,4,5]. Abdominal radiography cannot be used to exclude the diagnosis of AMI, once radiographic findings, such as PVG, are usually late and non-specific. [5]. The role of ultrasound in the diagnosis of AMI is limited due to the difficulty in the assessment of distal visceral vessels, the relative length of the examination, and the pain associated with the abdominal pressure required. [2,5]. CT angiography is the most appropriate imaging modality for the diagnosis of AMI, with a sensitivity and specificity of 93 and 100%, respectively. [5]. “Routine” CT with IV contrast may establish or suggest the diagnosis of AMI. Non vascular CT findings include hypoperfusion and hypoattenuation, bowel dilatation, intestinal pneumatosis, and PVG. Vascular findings include arterial stenosis, arterial embolism, arterial thrombosis and arterial dissection. [5]. The initial care of AMI includes fluid resuscitation as needed, serial management of acid-base status, and electrolyte levels, and early invasive hemodynamic monitoring. Medicines including heparin, antibiotics, and vasodilators can be successfully administered in patients who present with AMI. [2]. Treatment options for AMI are endovascular repair and open surgery. Open surgery is the most common approach, nevertheless, prognosis remains poor, with a short-term mortality ranging from 26% to 65%. Endovascular repair may be most appropriate for patients in which the ischemia is not severe and those with a high risk for complications and death associated with open surgery due to co-existing co-morbidities. [2].
Lista de Diferenciais
Diagnóstico
Aprendizado
In this report, we learned to watch out for patients who present a pain “out of proportion to the examination”, associated with symptoms such as confusion, tachypnea, tachycardia, vomiting and nausea. The imaging exams are very important in these cases to investigate a probable diagnosis of acute mesenteric ischemia, and also demonstrate signs of severity such as portal venous gas.
Referências
Kühn F, Schiergens TS, Klar E. Acute Mesenteric Ischemia. Visc Med. 2020 Aug;36(4):256-262. doi: 10.1159/000508739. Epub 2020 Aug 4. PMID: 33005650; PMCID: PMC7506269.
Clair DG, Beach JM. Mesenteric ischemia. N Engl J Med. 2016 Mar; 374:959–968. Doi: 10.1056/NEJMra1503884.
Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, Ben-Ishay O, Rubinstein C, Balogh ZJ, Civil I, Coccolini F, Leppaniemi A, Peitzman A, Ansaloni L, Sugrue M, Sartelli M, Di Saverio S, Fraga GP, Catena F Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg 2017;12:38
Magrach LA, Martín E, Sancha A, García M, Cendoya I, Olabarria I, et al. Gas venoso portal intrahepático. Significado clínico y revisión de la bibliografía [Hepatic portal venous gas. Clinical significance and review of the literature]. Cir Esp. 2006 Feb;79(2):78-82. Spanish. doi: 10.1016/s0009-739x(06)70824-7. PMID: 16539944.
Ginsburg M, Obara P, Lambert DL, et al. ACR Appropriateness Criteria Imaging of Mesenteric Ischemia. J Am Coll Radiol. 2018 nov;15(11):S332-S340. doi:10.1016/j.jacr.2018.09.018.
Imagens

Figure 1: CT, arterial phase, coronal image shows acute occlusion in the superior mesenteric artery (yellow arrow).
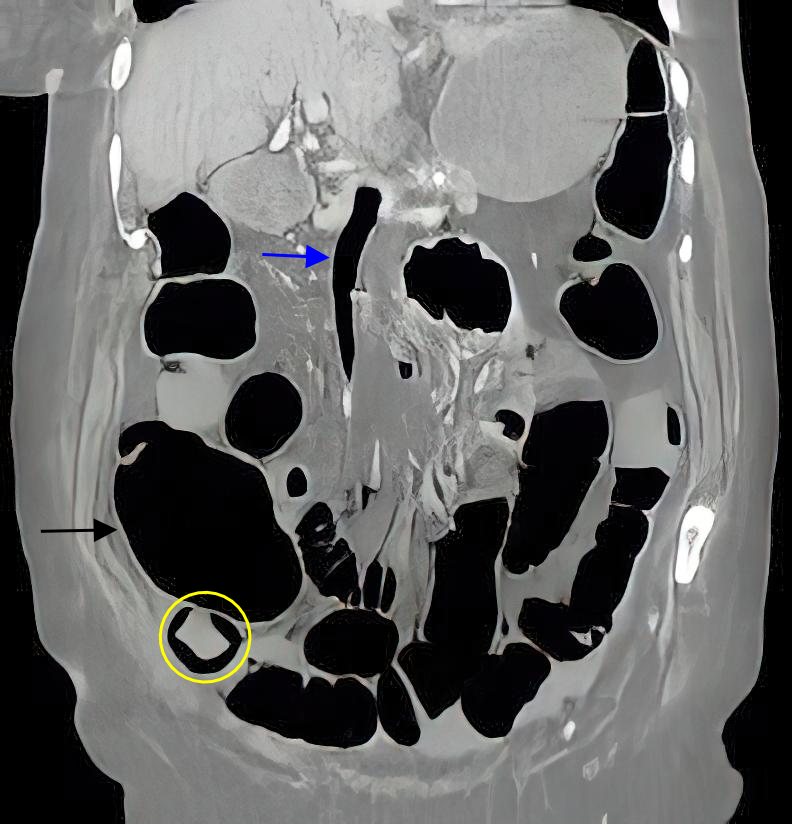
Figure 2: CT, portal venous phase, coronal image demonstrates gaseous distension of intestinal loops (black arrow), air inside the superior mesenteric vein (blue arrow), and pneumatosis in the ileum (yellow circle).
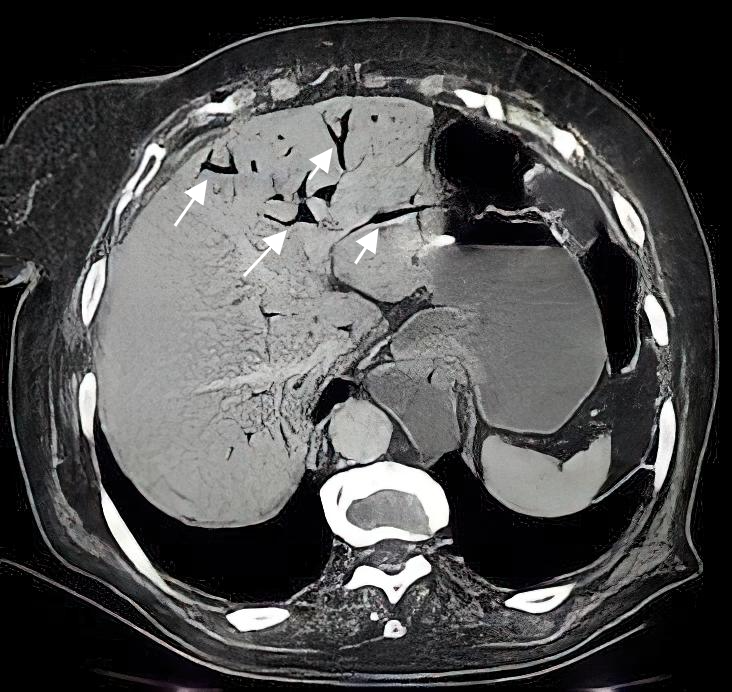
Figure 3: CT, portal venous phase, axial image shows air in the portal vein branches (white arrows).
Artigo recebido em quarta-feira, 9 de junho de 2021
Artigo aprovado em quinta-feira, 11 de novembro de 2021
 Todos os artigos científicos publicados em brad.org.br são licenciados sob uma licença Creative Commons.
Todos os artigos científicos publicados em brad.org.br são licenciados sob uma licença Creative Commons.