André Vaz 1, Pietro Bosquirolli Maffezzolli 2
Abstract
We report a case of hemorrhagic cystitis after bone marrow transplant.Dados do caso
Feminino 13 anos
Palavras chaves
Cistite, Transplante de Medula Óssea, Hematúria
Histórico Clínico
A 13-year-old girl on the 53rd day after bone marrow transplant (BMT) presented dysuria and fever. Broad-spectrum antibiotic therapy was initiated, however, there was no bacterial growth in blood or urine cultures. After 3 days, she started with macroscopic hematuria. Urine adenovirus screening was negative and polyomavirus screening was positive.
Achados Radiológicos
Bladder with reduced capacity and marked parietal thickening, especially of the anterior and superior walls.
Discussão
Hemorrhagic cystitis (HC) is considered a frequent complication of BMT, which can occur in up to 66% of these patients, especially those who underwent allogeneic transplantation [1-6]. HC is classified in early and late types according to the BMT date. Early type HC occurs up to 7-9 days [1,4] after the BMT and results from toxicity of the conditioning regimen [1,3,6]. Late type HC occurs between 2 weeks and 6 months after the BMT and may result from viral infection [1-6] or graft versus host disease [2]. Among the infectious causes, the main etiologies are BK palyomavirus (BKV - 80.8%), adenovirus (15.4%) JC virus (3.8%), cytomegalovirus and, rarely, simian virus SV40 [1-6]. The main cause of late HC is related to BKV [3]. Primary infection of BKV is believed to occur in early childhood and may cause a self-limiting respiratory tract disease [5,6]. The infection remains latent in immunocompetent hosts, however, when in a immunosuppression state, there may be a reactivation of viral replication which may progress to nephropathy or ureteral stenosis in kidney transplant recipients or HC in BMT recipients [3,5,6]. The diagnostic criteria for BKV-associated HC consist of: cystitis symptoms (dysuria, hypogastric pain), macroscopic hematuria and viruria greater than 7 log copies/mL [1]. Although not essential for the diagnosis, the main role of imaging is the characterization of urinary bladder hematoma that may indicate irrigation. Other imaging findings include: reduced bladder capacity, continuous or discontinuous bladder wall thickening (notable predominance in the anterior wall), which may be accompanied by hypervascularization on color Doppler or parietal enhancement and perivesical adipose tissue densification in computed tomography [3,5,6]. Most cases resolve in 3 to 5 weeks with supportive therapy and antiviral therapy with Cidofuvir is controversial, due to lack of evidence of its benefit [1].
Lista de Diferenciais
Diagnóstico
Aprendizado
Teaching Points: - Hemorrhagic cystitis is classified in early and late types; - Early type HC (< 1 week after BMT) results from toxicity of the conditioning regimen; - Late type HC (2 weeks to 6 months after BMT) results from viral infection or graft versus host disease; - Cystitis symptoms, macroscopic hematuria and viruria are the main findings of BKV-associated HC diagnosis; - The main role of imaging is to recognize intravesical clots.
Referências
Imagens
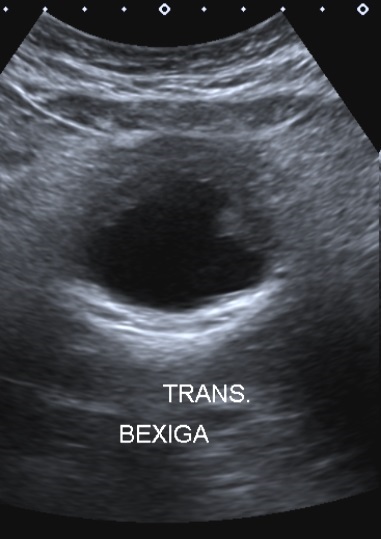
Ultrasonography of the bladder in the transverse plane demonstrating reduced capacity and marked thickening and irregularity of the anterior wall.
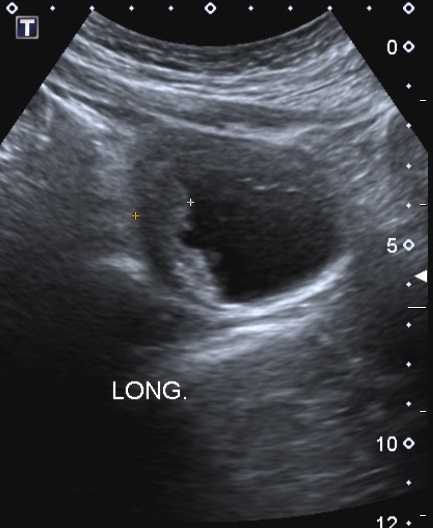
Ultrasonography of the bladder in the midline longitudinal plane demonstrating reduced capacity and marked thickening and irregularity of the anterior and superior wall.
Vídeos
Article receive on Wednesday, March 25, 2020
Artigo aprovado em Monday, March 30, 2020
 All scientific articles published at brad.org.br are licensed under a Creative Commons license.
All scientific articles published at brad.org.br are licensed under a Creative Commons license.